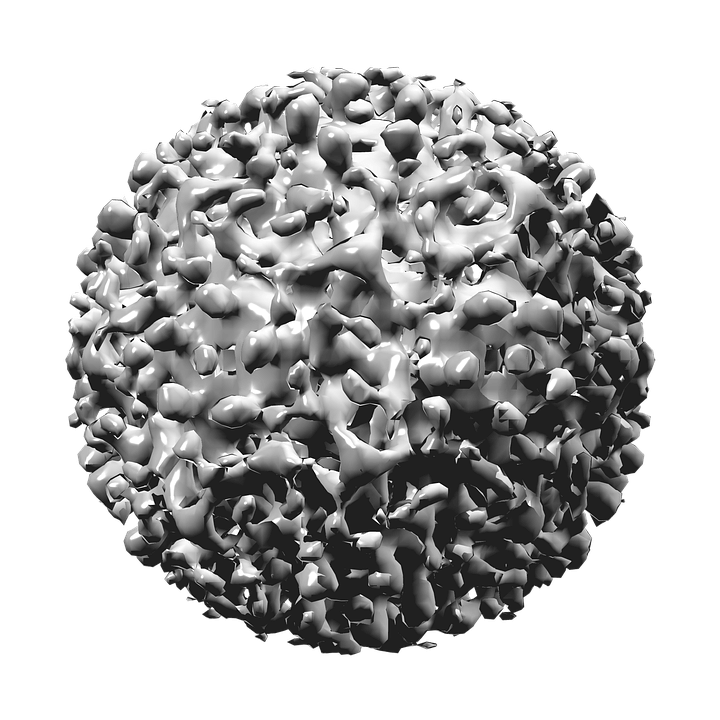
Hepatitis B virus (HBV) infection is a serious illness in the newborn and young infant. The virus, first discovered in the mid-1960s, is transmitted through percutaneous (i.e., puncture through skin) or mucosal (i.e., direct contact with mucous membranes) exposure to infectious blood or body fluids. The virus is highly infectious, can be transmitted in the absence of visible blood, and remains viable on environmental surfaces for at least seven days. Once the virus enters the body, it is transported to the liver where it replicates. Although one generally thinks of the acute illness as a self-limited one in the adult with characteristic signs and symptoms, HBV infection in the infant is almost exclusively asymptomatic and hence, unrecognized. The devastating aspect of the infection is that the infant and young child frequently fail to clear the virus, and the illness becomes chronic. As many as 80-90% of infected infants progress to chronic infection, and chronically infected persons as adults are at increased risk of cirrhosis, hepatocellular carcinoma, and liver failure with approximately 25% dying from these serious complications.
Before 1982, an estimated 200,000-300,000 persons in the U.S. alone were infected with HBV annually, including approximately 20,000 infants. No effective pre-exposure prophylaxis existed, and only post-exposure prophylaxis in the form of hepatitis B immune globulin (HBIG) was available. However, the first hepatitis B vaccine was approved in the United States in 1981 and proved to be a real game changer. The availability of the vaccine set the stage for remarkable progress in the elimination of HBV infection among all age groups. With the advent of an effective vaccine, incurable hepatitis B infection had become preventable. The vaccine saves lives!
It is in this setting of disease prevention through widespread vaccination that an evolving strategy to eliminate perinatal hepatitis B infection was initiated over 30 years ago. Early epidemiological studies had demonstrated that a major contributor to perinatal HBV infection is mother-to-child transmission (MTCT) at the time of delivery. In utero infection is felt to account for less than 2% of infections. The risk of transmitting the virus was estimated to be 20-80% depending on the activity of the maternal infection. Initial attempts in the early 1980s to limit vertical HBV transmission were risk-based and aimed at identifying those pregnant women considered infectious by virtue of the serum marker, HBsAg. With reliable identification of mothers and expeditious treatment of their newborns with hepatitis B vaccine and HBIG, HBV infection could be prevented. However, it became clear within several years that such screening was inadequate with as many as 35-65% of HBsAg-positive women being missed. Consequently in 1988, the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention recommended universal testing of all women early in each pregnancy such that at risk babies would receive appropriate post-exposure HBV prophylaxis. Throughout the 1990s, efforts were intensified to eliminate all HBV-related illness through widespread vaccination of children, adolescents, and at-risk adults. Studies showed that receipt of the 3-dose hepatitis B vaccine series produced a protective antibody response in approximately 98% of healthy infants. During 1990-2004, the incidence of acute hepatitis B in the U.S. declined by 75%. The greatest decline (94%) occurred among children and adolescents, most likely due to increasing hepatitis B vaccine coverage. As of 2004, over 92% of children less than 3 years of age had been fully vaccinated with the complete series.
Coupled with the remarkable success of the hepatitis B elimination strategy is the knowledge that the task is not complete. As a response to the persistence of perinatal HBV infection and aware that errors in testing as well as in communication of results may occur, ACIP has recommended a change in the administration of the initial hepatitis B vaccine dose over time. Initially, the first dose could be administered to an infant born to a HBsAg-negative mother any time from birth to 2 months of age. Subsequently the initial dose became the “birth dose” with the recommendation that it be given prior to discharge, and in 2017, the initial dose was to be administered within 24 hrs of birth. The previous permissive language that allowed the dose to be delayed “on a case-by –case basis and only in rare circumstances” was omitted. Based on the fact that the vaccine alone is 75% effective in preventing MTCT, these changes reflect reality and provide basic protection. Then too, the emerging concept that maternal viral load (HBV DNA) plays a significant role in risk of MTCT now plays a prominent role in management. Testing pregnant HBsAg-positive women for HBV DNA is now recommended to guide the use of antiviral therapy during the third trimester for the purpose of preventing perinatal HBV transmission.