Though it is not an incredibly common diagnosis, there are still thousands of fetuses diagnosed with an echogenic bowel each year. Roughly 1.8 percent of all fetuses have echogenic bowel, and their parents often wonder what exactly this term means. Understanding all the details about echogenic bowel will help parents discover how to handle this condition.
What Is Echogenic Bowel?
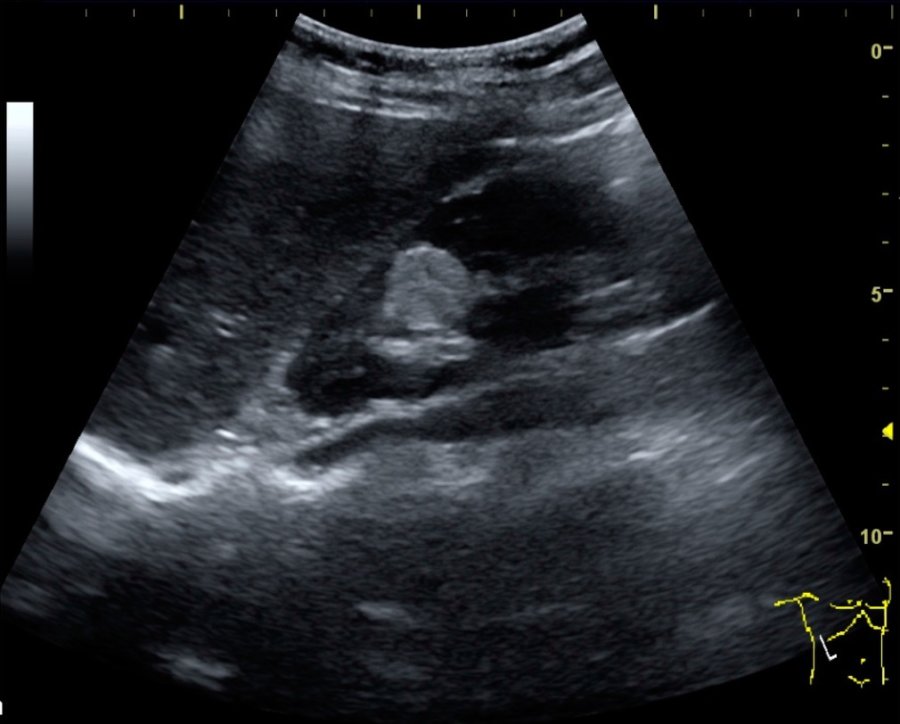
This term is simply used to refer to a fetal bowel that is abnormally bright when viewed on an ultrasound. Ultrasounds are always in shades of black, grey, and white, with denser tissue being bright white and fluid being black. Usually, the bowels of the fetus tend to be a dark grey on an ultrasound because they are softened tissue, but if a fetus has echogenic bowel, their bowels may look as bright as thick bones like the pelvic bone.
What Does It Mean to Have Echogenic Bowel?
When parents first hear this word, they often start to wonder if it is a serious problem. The reality is that it is not always a sign of a health condition. 0.5 percent of all perfectly healthy fetuses have an echogenic bowel, and it can just occur due to various fluctuations in growth. However, echogenic bowel can be a cause for concern because it is more common in babies born with Down syndrome or cystic fibrosis. It can also be a sign that the fetus is suffering from an intestinal obstruction or an infection like cytomegalovirus or toxoplasmosis.
How Is Echogenic Bowel Treated?
The method for addressing echogenic bowel typically depends on the severity. Low grade echogenic bowels which are less dense than bone are normally harmless, so doctors tend to take a “wait and see” approach. They normally recommend taking a more detailed ultrasound in a few weeks to check up on the growth of the fetus. However, for more severely echogenic bowels, doctors may recommend a maternal serum screening, blood tests, or an amniocentesis to determine if the fetus has Down syndrome, infections, or cystic fibrosis. To make sure that the pregnancy continues safely, doctors will usually do regular fetal monitoring to make sure the fetus is growing properly following a display of echogenic bowel.