A tetralogy is a cluster of four abnormalities or symptoms that exist at the same time. Tetralogy of Fallot is a condition where four separate genetic heart issues occur in the same person.
A tetralogy is a cluster of four abnormalities or symptoms that exist at the same time. Tetralogy of Fallot is a condition where four separate genetic heart issues occur in the same person.
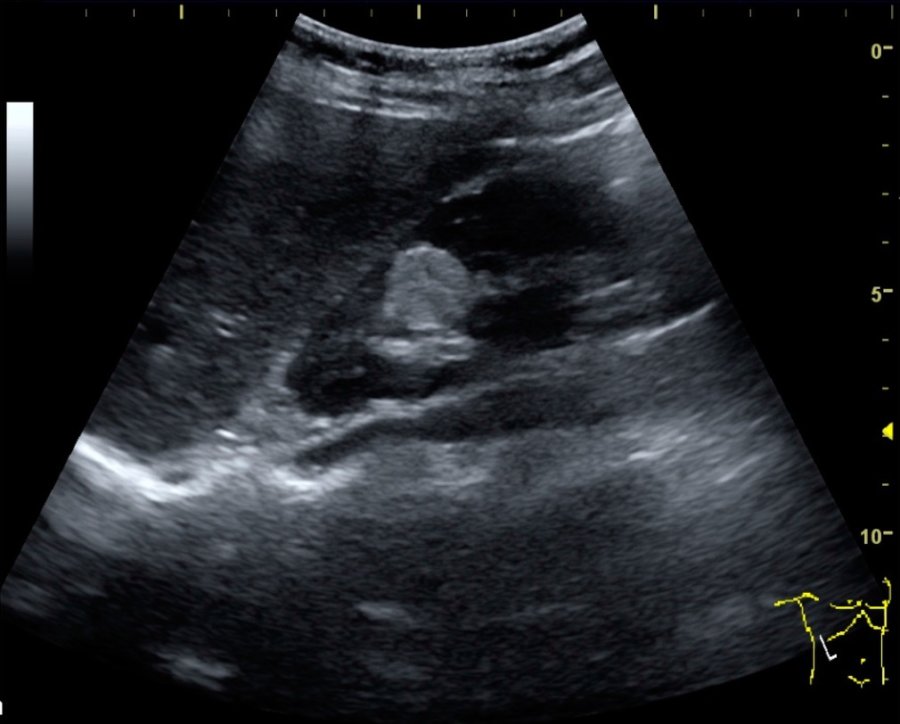
They are a hole between the lower chambers of the heart, or ventricular septal defect. Pulmonary valve stenosis, or a narrowed pathway between the heart and lungs, is another. An overriding aorta means that the aorta is positioned over the hole in the lower chambers. Finally, right ventricular hypertrophy means that the muscle that encases the lower right chamber becomes unusually thick. This is a serious issue because it makes it more likely the heart will become stiff and go into failure.
Usually, Tetralogy of Fallot is diagnosed in small babies. It’s a rare condition, but some of the symptoms are very distinctive. This cluster of symptoms causes oxygen-poor blood to circulate from the heart to the body. As a result, babies with it sometimes have a bluish appearance. This is also known as cyanosis.
Tetralogy of Fallot can vary in degree of severity. It often co-occurs with Down Syndrome or DiGeorge Syndrome. There are children who have other heart defects in addition to the ones in the tetralogy. Some people with less severe forms of this condition aren’t diagnosed until adulthood. Their symptoms can include fainting, clubbed fingers and toes and shortness of breath.
The treatment for Tetralogy of Fallot is surgery. There are two different ways medical teams approach this. Sometimes in babies, the first operation performed is only a temporary one. This can depend on how complicated the case is and what other problems may be present. Later on, a complete repair is completed. In cases with no complicating factors, the first operation may be the permanent, complete one.
Some people who have the surgery will need to see a cardiologist who has extensive experience with congenital defects throughout their lives. Sometimes, follow-up surgeries are required after the first repair procedure. These can include stent surgeries. The causes of Tetralogy of Fallot are mysterious. Sometimes, an infection like rubella can be to blame. At other times, it may be related to dietary deficiencies. There may also be a genetic component.